Tomorrow, the new 988 crisis line for mental health and substance use emergencies goes live across the country. Approximately one year ago, The Kennedy Forum shared an analysis of state legislative action needed to support 988 by the national go-live date. At the time, only Colorado, Nevada, and Washington had passed adequate legislation to facilitate 988 implementation (i.e. having a comprehensive plan for a full behavioral health crisis continuum and ongoing funding to see the systems—call centers staffed by mental health professionals, mobile response teams, and crisis stabilization services—built out). Unfortunately, no other states have been added to this list to date. As it stands now, less than 8% (24.7 million) of the population are in states that have passed needed legislation.
A deeper dive into state activity
Eighteen states have introduced 988 fee legislation that have not moved forward. Some bills have set fee amounts that are insufficient to fund needed services, while others have been downgraded to “study bills” or unfunded 988 “processes.”
Between February and July of 2022, five states had 988 fees actively stripped out of their bills in part because telecom companies opposed the funding mechanism the federal government authorized, which would allow them to pass a “user fee” on phone lines that would fund comprehensive implementation of 988.
As of July 2022, California is the only state still considering a comprehensive fee and planning process. In preparation for the go-live date, The Kennedy Forum, in partnership with Steinberg Institute, NAMI California, NAMI Contra Costa, Mental Health America of California, The Miles Hall Foundation, Contra Costa County, Los Angeles County, and the California Council of Community Behavioral Health Agencies (CCCBHA), successfully advocated for the necessary funding and appropriations to support 988. We are happy to report that California has approved the following:
- Funding for call centers for year one operations ($8 million)
- $7.515 million for start-up funding and an additional $5.975 million for ongoing funding to implement technical components of 988 and 911-988 interoperability
- A new Medicaid benefit that allows a federal match of 85% for mobile crisis intervention services (this means the state will allocate $1.4 billion for these services, the federal government will then match 85%, leaving the remaining $335 million to be covered by state funds during the duration of this benefit)
- Additional funding through two specific programs: the Behavioral Health Continuum Infrastructure Program and the Behavioral Health Crisis Continuum Planning program, both of which would build out comprehensive crisis stabilization services
If passed, AB 988 would establish a fee of $0.08 for the first two years to sustain 988 call center operations and support a comprehensive state planning process. The fee would then be set based on system needs every year thereafter, just as the state’s 911 system is currently funded, with a cap of $0.30. The bill’s bipartisan support (70-0 in the Assembly, and 12-0 and 10-0 in Senate committees) is a remarkable indicator that this model works on both sides of the aisle.
The majority of the U.S. still has a long way to go—92% of the population live in states without a comprehensive plan and sustainable funding structure for 988. Nevertheless, with federal guidance and legislation from other states like California as a guide, we can continue to make progress. It’s time to pivot from a planning mindset to a catch-up mindset.
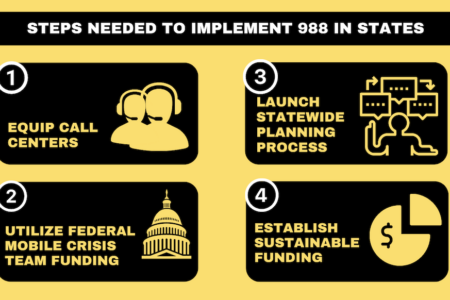
The following actions must be taken by remaining states as soon as possible:
- Ensure 988 call centers are equipped to respond. Current crisis call centers will likely need to handle an increase in volume. States should act swiftly to ensure National Suicide Prevention Lifeline-designated crisis call centers are staffed and funded.
- Take advantage of federal mobile crisis team funding. While call centers facilitate remote care, they must also be able to refer people to in-person crisis services through mobile crisis teams. Through state plan amendments or within waiver authorities, states can draw down an enhanced 85% federal medical assistance percentage (FMAP) for mobile crisis services for 12 quarters within a five-year period. Centers for Medicare and Medicaid Services (CMS) recently issued guidance outlining this and additional considerations on reimbursement for mobile crisis services.
- Launch a statewide planning process. With immediate funding needs secured for call centers and a large portion of mobile crisis teams, states must also consider long-term planning for a sustainable process to connect all components of the crisis system. This includes technical operations between 911 and 988, local and county behavioral health agencies, call centers, and crisis services. The Substance Abuse and Mental Health Services Administration’s National Guidelines for Behavioral Health Crisis Care offers a helpful roadmap for states on clinical best practices.
- Establish sustainable funding. To ensure funding of a 988 system build-out, states can establish a fee on phone lines for these services, as outlined in the federal legislation, and/or can appropriate other funds including ongoing general fund revenue.
Now is the moment for states to demonstrate their commitment to ending discrimination against those with mental health and substance use disorders. Far too many individuals, families, and communities have suffered due to systematic failures in recognizing and addressing crisis.
Compassion, understanding, and informed decision-making must guide all efforts moving forward.
To track 988 legislation by state, see NAMI’s Reimagine Crisis Map. To view model 988 legislation, see the National Association of State Mental Health Program Director’s suggested language.